Help Edward Find a Kidney
Hi, my name is Edward Hilgendorf, and this is my story of living with CKD, chronic kidney disease.
In late 2018 I started feeling very ill, I was having a hard time focusing and remembering what was happening. I felt weak, tired and often found myself confused.
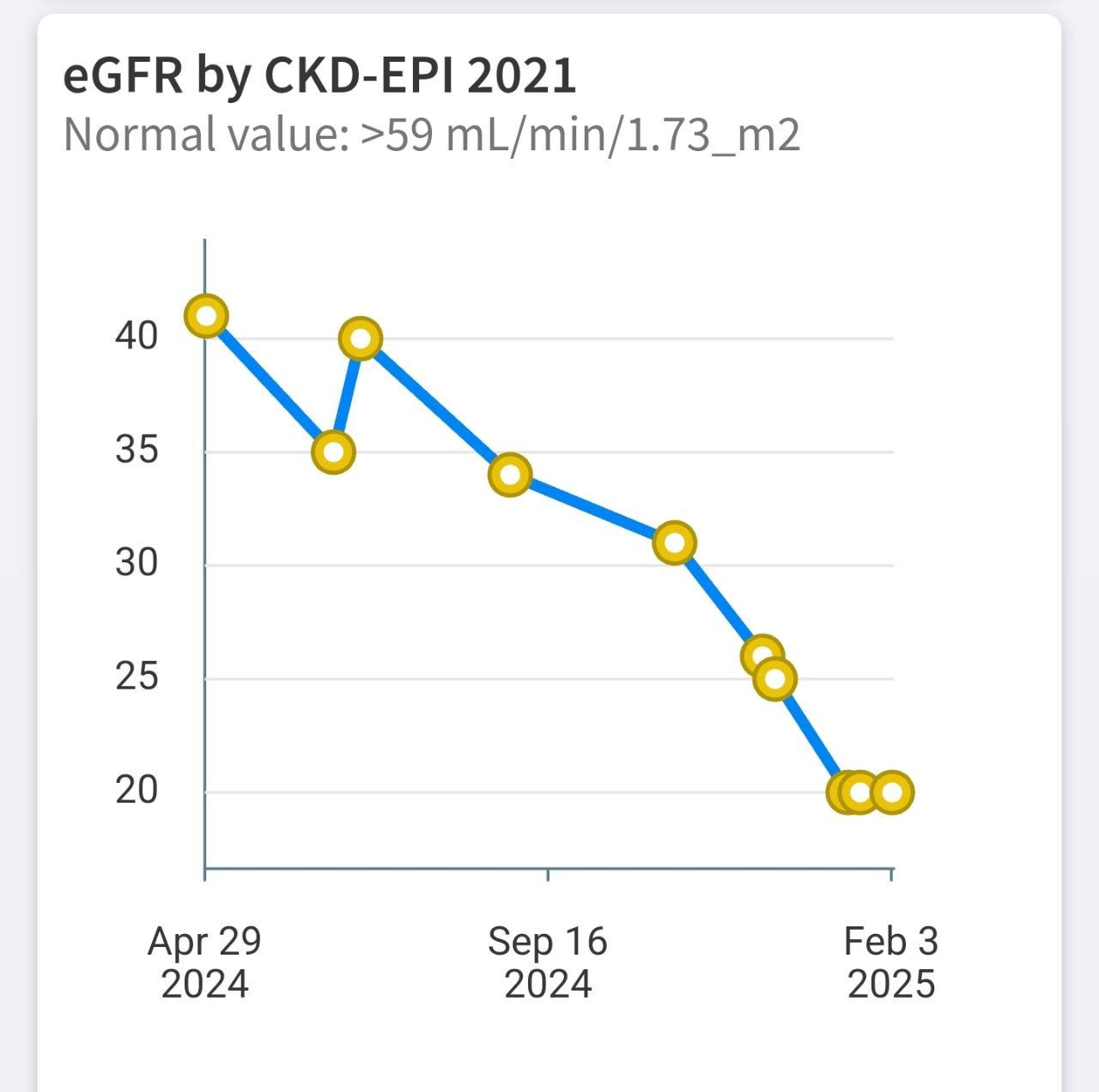
I visited an urgent care who after a quick evaluation determined I was likely fine, but requested full labs to be sure, which resulted in me finding I was in Stage 4 of kidney disease with an eGFR of 24.
My amazing team at the University of Washington quickly started me on medication, primarily blood pressure medication, with my blood pressure being 160+ over 100 on average. Blood pressure has a cyclical relationship with kidney function -- the higher your blood pressure, the faster the kidney declines, and the worse the blood pressure gets.
After an intense week in the hospital of scans and biopsies, I was diagnosed with IGAn, or IGA Nephropathy. IgA nephropathy is when your immune system mistakenly attacks your kidneys -- the more it attacks, the more kidney damage occurs, and the worse your immune system gets at telling friend from foe.
I was told I needed to seek a transplant immediately. I am very blessed to have an amazing family and support system, nearly everyone in my family got tested to be a match, and my brother was a remarkable 100% match with me. They told me I would have likely never be sick again, and I would live a completely normal life, as with such a high match you need very little immunosuppressive medication, which is the only real downside to receiving a kidney transplant.
We went through months of testing to be sure we would both be suitable, but at one point my function dropped dramatically from around 20% at which point I was still able to live a somewhat normal life, to less than 14%, which is stage 5 kidney disease, or, end stage renal failure.
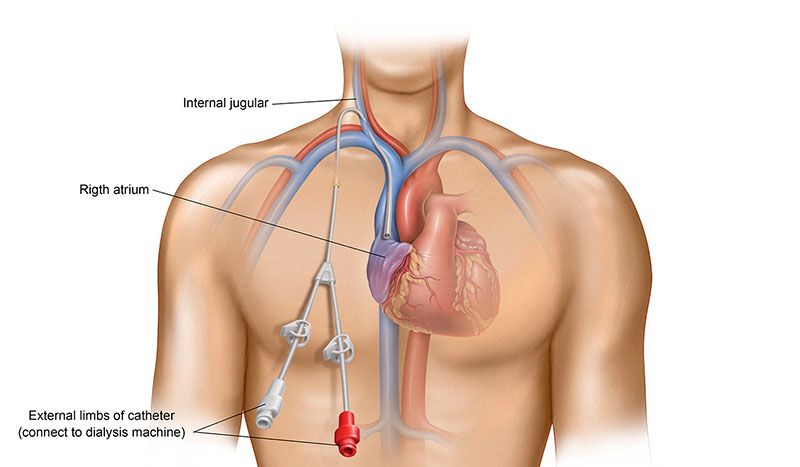
The only option I had until the transplant date was emergency dialysis via a central venous catheter. A CVC catheter is a large tube inserted into a major vein near your heart -- it gives direct access to your bloodstream for treatments like dialysis, but the bigger the access, the higher the risk of serious infections and blood clots. It's not a solution, but a temporary band aid.
This was my first introduction to dialysis. Dialysis is an artificial kidney machine that cleans your blood when your kidneys can't -- it removes waste and excess fluid, but the longer you need it, the more your remaining kidney function tends to decline. The CVC is connected to lines that go to a large machine, a cycler with multiple filters. Your blood gets removed, the waste and water removed, then put back into your body.
I stayed in the hospital for a couple weeks on dialysis, my transplant surgery was rushed because a CVC is incredibly risky to keep. This surgery went well, everything went as planned, except when I woke up, I could no longer empty my bladder. This was a major red flag, as the success of kidney transplant is measured by your ability to urinate. Your kidneys are like filters that pull waste and extra water from your blood to create urine, so when they're severely damaged, that filtering process breaks down. But I had a brand new, healthy kidney, my team immediately investigated with a biopsy, and confirmed that my newly transplanted kidney was not yet functioning. Unfortunately, the biopsy did not go as planned and after a day I had intense pain in the newly transplanted kidney. The biopsy caused a hematoma on the new kidney, which escalated to ischemia. I needed an emergency repair surgery, and was rushed to the OR. I woke up in the ICU, where I spent the next two eeeks on dialysis. These were the hardest two weeks of my life.
On dialysis your blood pressure crashes, you constantly experience intense muscle cramps when the machine removes too much water from you, constant nausea, and exhaustion that can lasts for hours. For the next few weeks I stayed in the hospital with two constant sounds as reminders: the hum of the dialysis machine, and the shouts for help from other dialysis patients in excruciating pain from cramps.
After a couple weeks, something amazing happened -- I had to urinate for the first time in almost a month. My new kidney had woken up. I immediately felt better than I had in years. They tested my function -- my eGFR was over 60, or essentially almost no kidney disease. My CVC was removed -- an experience that will haunt my wife and I for the rest of our lives as the nurse pulled the line as if she was starting a lawn mower, accompanied by a tearing sound followed by an loud pop as the line was removed, and immediately placing a large bandage on my chest with as much pressure as possible. I would no longer need dialysis.
Over the next 4 years I did everything I wanted -- I backpacked in the pacific northwest, swam in the ocean, kayaked, traveled to Colombia to visit family, traveled across the United States, hiked, bicycled, and everything I was unable to do before, and I felt wonderful the entire time.
In 2023, seemingly out of nowhere, on a routine blood draw, my results showed that my eGFR was now 53, not over 60. We continued to test bi-weekly, and saw it continue to fall. I trialed numerous drugs over this time, anything that may stop the IGA from recurring, to no avail. By December of 2024, I was back again at stage 4 CKD, where I had started, with a GFR of 24. The recurrent IGA had permanently scarred my new kidney, and I was in need of a transplant. What was meant to last a lifetime, lasted around 5 wonderful years that I will never forget. I think about my brother every day as I do something I would not have been able to do.
In December a trial medication by the name of Iptacopan had passed FDA testing became available, this medication was the first IGA specific medication on the market that has shown to significantly slow down kidney failure progression, and in some cases, raise kidney function back to a normal level. Unfortunately for me, I already had too much permanent damage, but amazingly enough, this drug has kept me in stage 4 for six full months without progressing to stage 5.
I am now on the cusp of end stage failure, my GFR is 18, and my doctors are asking me to mentally prepare me for dialysis. I have had frequent sleepless nights where I wake up soaked in sweat after a nightmare of being back in the hospital and hearing the dialysis machine, accompanied by the beep of a heart rate monitor, and the screams of other dialysis patients experiencing dialysis muscle cramps.
To make matters worse, while I was being tested to see if I would again be a candidate for another transplant, the doctors found a mass that had grown to 5cm on my native kidney. It was kidney cancer, but luckily, highly likely to be stage 1, and treatable by a nephrectomy, where they will remove the native, non-functioning kidney.
With the contingency of successful cancer removal, I have been again approved for a kidney transplant and I am accruing my time on UNOs for a deceased kidney: https://unos.org/. The wait time is 3 to 5 years, but can be longer with rare blood types like mine, B-.
I am hoping that I will find another living donor match (patients with a living donor have the highest chance of survival), and with the combination of that and this new medication (Iptacopan), I will have a long, healthy life.
If you've ever considered becoming a living kidney donor, please take a moment to learn more.
To learn more about dialysis, please see this video from John Oliver: https://www.youtube.com/clip/UgkxZdNO855rFnovWDHTTsNZy5XcNMTO4T8K.
Learn More About Donation
UW Medicine Living Kidney Donor Program National Kidney Foundation: Becoming a Living DonorFind Out If You Are a Match
Find Out If You Are a MatchThank You
Your consideration means the world to me. If you're interested in donating or have any questions, please reach out.